Breast cancer is defined by the unchecked expansion of abnormal cells in the glands that produce milk in the breast or in the ducts that carry milk to the nipples. It may start in the breast lobules or ducts. Breast tumors often grow slowly. A lump could have been developing for up to 10 years before it becomes large enough to feel.
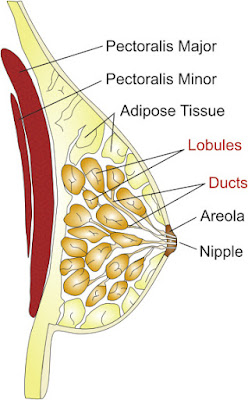
Structure of Breast
Early prevention of Breast cancer
One of the newest ways to protect yourself is to learn whether you have dense breasts. When you have more tissue than fat in your breasts which is common in younger women – it makes cancer harder to detect on a mammogram: Both tumors and breast tissue show up white, while fat looks dark.
Exercise seems to protect against it in several ways. First, it helps control weight.
Know your family cancer history – even your dad’s. If your family history worries you, enlist the help of a genetics expert.
Minimize radiation exposure from screening tests. Ionizing radiation—the kind in many high-tech screening tests—is a risk factor for the disease, because ionizing radiation can cause DNA mutations in cells.
Describes a cancer that has not spread beyond the ducts or lobules where it began. Ductal carcinoma in situ (DCIS) is a type of non-invasive breast cancer. DCIS occurs when abnormal cells grow inside the milk ducts, but have not spread to nearby tissue or beyond. The term “in situ” means “in place.” Although the abnormal cells have not spread to tissues outside the ducts, they can develop into invasive breast cancer.
Invasive breast cancer or metastatic breast cancer
Occurs when abnormal cells from inside the milk ducts or lobules break out into nearby breast tissue. Cancer cells can travel from the breast to other parts of the body through the blood stream or the immune system. They may travel early in the process when the tumor is small or later when the tumor is large.
The most common types of breast cancer
The type of breast cancer is important in determining the most effective treatment approach. The most common way to classify breast tumours is according to the status of three specific cell surface receptors. These are:
The oestrogen receptor (ER)
The progesterone receptor (PR) and
The Human Epidermal Growth Factor Receptor (HER)2/ neu receptor
1. Hormone Receptor-Positive breast cancer
This type of cancer grows in response to the hormones oestrogen and progesterone, and as such is likely to respond to therapies that aim to inhibit the growth effects of hormones.
2. HER2-positive breast cancer
HER2-positive breast cancer which is typified by cells that make too much of a protein known as HER2/neu. It represents 20–30% of Hormone Receptor Positive breast cancers. Tumors that do not overexpress HER2/neu are described as HER2-negative.
3. Triple negative breast cancer (TNBC)
Triple negative breast cancer (TNBC) is a rarer form of breast cancer which is a sub-type of HER2-negative disease. TNBC refers to tumour cells which lack oestrogen and progesterone receptors, and do not overexpress the HER2 protein. This cancer type accounts for around 15% of all breast cancers, and is usually more aggressive and difficult to treat as it does not tend to respond to standard therapies.
Breast cancer stages
Pathologic staging (the standard way to stage breast cancer) is based on a pathologist’s study of the tumor tissue and any lymph nodes removed during surgery.
TNM system of staging
Although there are a few ways to classify stage, the most widely used is the TNM system.
TNM stands for:
T = Tumor size
N = Lymph Node status (the number and location of lymph nodes with cancer)
M = Metastases (whether or not the cancer has spread to other areas of the body)
Stage 1
This is divided into two groups: A and B.
Stage 1A means: The cancer is 2cm or smaller and hasn’t spread outside the breast.
Stage 1B can means: No cancer is seen in the breast, but a few cancer cells are found in the lymph nodes under the arm (known as micro metastasis) (OR) The cancer in the breast is 2cm or smaller and a few cancer cells are found in the lymph nodes under the arm (micrometastasis).
Stage 2
This is divided into two groups: A and B.
Stage 2A can mean: No cancer is seen in the breast but cancer is found in one to three lymph nodes under the arm or near the breastbone (OR) The cancer in the breast is 2cm or smaller and cancer is found in one to three lymph nodes under the arm or near the breastbone (OR) The cancer in the breast is larger than 2cm but smaller than 5cm and no cancer is found in the lymph nodes under the arm.
Stage 2B can mean: The cancer in the breast is larger than 2cm but smaller than 5cm. Cancer is found in one to three lymph nodes under the arm or near the breastbone (OR) The cancer in the breast is larger than 5cm and no cancer is found in the lymph nodes under the arm.
Stage 3
This is divided into three groups: A, B and C.
Stage 3A can mean: No cancer is seen in the breast, but cancer is found in four to nine lymph nodes under the arm or near the breastbone (OR) The cancer in the breast measures up to 5cm and cancer is found in four to nine lymph nodes under the arm or near the breastbone (OR) The cancer in the breast is larger than 5cm, and cancer is found in up to three lymph nodes under the arm or near the breastbone.
Stage 3B means: The cancer in the breast can be any size and has spread to the skin of the breast or chest wall. Cancer is found in up to nine lymph nodes under the arm or near the breast bone.
Stage 3C means: The cancer in the breast can be any size, may have spread to the skin of the breast or chest wall and cancer is found in 10 or more lymph nodes under the arm or near the breastbone, or to nodes above or below the collarbone.
Stage 4
The cancer can be any size, the lymph nodes may or may not contain cancer, but the cancer has spread (metastasised) to other parts of the body, such as distant lymph nodes, lungs, bones, liver or brain.
If your cancer is found in the lymph nodes under the arm but nowhere else in the body you do not have stage 4.
Historical view
In ancient Greece, people made votive offerings in the shape of a breast to the god of medicine. And Hippocrates described the stages of breast cancer in the early 400s B.C.E. In the first century A.D., doctors experimented with surgical incisions to destroy tumors. They also thought that breast cancer was linked with the end of menstruation. This theory may have prompted the association of cancer with older age.
In the beginning of the Middle Ages, medical progress was linked with new religious philosophies. Christians thought surgery was barbaric and were in favor of faith healing. Meanwhile, Islamic doctors reviewed Greek medical texts to learn more about breast cancer.
The Renaissance saw a revival of surgery as doctors began exploring the human body. John Hunter is known as the Scottish father of investigative surgery. He identified lymph as a cause of breast cancer. Lymph is the fluid carrying white blood cells throughout the body. Lumpectomies were also performed by surgeons, but there was no anesthesia yet. Surgeons had to be fast and accurate to be successful
Prevalence of breast cancer
Worldwide: Globally, over one million women are diagnosed with breast cancer every year. It is the most frequently diagnosed cancer in women and the leading cause of cancer death in women. Every year more than 500,000 women die from the disease.
Europe: In Europe over 400,000 women are diagnosed with breast cancer every year and 120,000 women die from the disease. It is the most frequently diagnosed cancer in Europe and the leading cause of cancer death in European women. It accounts for 17% of female cancer deaths in this region.
North America: Over 200,000 women are diagnosed with breast cancer every year in North America. It is the second most deadly form of cancer in North American women after lung; it kills over 45,000 women a year, representing almost 15% of female cancer deaths in North America.
Risk Factors and causes
There are a number of factors that have been shown to increase a woman’s risk of developing it:
Age: The majority of breast cancer cases occur in women over the age of 50.8. Starting menopause after age 55. Never giving birth, or being older when your first child is born.
Family history: If a woman has a personal or family history of breast cancer she is at increased risk of developing breast cancer.
Clinical history: Women who have previously suffered with benign breast cancer are at greater risk of developing breast cancer in the future.
A late first pregnancy: Women who have a late first pregnancy (after the age of 35) are more likely to develop breast cancer.
Prolonged hormonal exposure: A long menstrual life or possibly use of hormone replacement therapy after the menopause expose women to an increased risk of developing breast cancer.
Lifestyle factors: For example, being overweight or obese after the menopause, physical inactivity, a high fat diet and high alcohol consumption can play an important role in the development of breast cancer
Being overweight, especially after menopause.
Taking oral contraceptives (birth control pills).
Signs and symptoms
Some warning signs are:
New lump in the breast or underarm (armpit).
Thickening or swelling of part of the breast.
Irritation or dimpling and bumps like of an appearance of breast skin.
Redness or flaky skin in the nipple area or the breast.
Pulling in of the nipple or pain in the nipple area.
Nipple discharge other than breast milk, including blood.
Pain in the breast.
A change in the size or shape of the breast, including indentation, ‘growing’ (particularly prominent) veins or skin erosion.
Diagnosis and Testing
Biopsy:
Fine Needle Aspiration (FNA): A thin needle is placed into the lump. If fluid comes out, and the lump disappears, it means that the lump is a cyst and is usually not cancer.
Core Biopsy: A larger needle is used to remove a small piece of tissue from the lump.
Surgical Biopsies: An incisional biopsy removes only a portion of the lump. An excisional biopsy removes the entire lump.
Lab tests
Hormone receptor tests: Some breast cancers need hormones to grow. These cancers have hormone receptors for the hormones estrogen, progesterone, or both. If the hormone receptor tests show that it has these receptors, then hormone therapy is often recommended as part of the treatment plan.
HER2 test: Some breast cancers have large amounts of a protein called HER2, which helps them to grow. The HER2 test shows whether a woman’s breast cancer has a large amount of HER2. If so, then targeted therapy against HER2 may be a treatment option.
Staging tests
Lymph node biopsy: If cancer cells are found in a lymph node, then cancer may have spread to other lymph nodes and other places in the body. Surgeons use a method called sentinel lymph node biopsy to remove the lymph node most likely to have breast cancer cells.
CT scan: You may receive contrast material by mouth and by injection into a blood vessel in your arm or hand. The contrast material makes abnormal areas easier to see. The pictures from a CT scan can show cancer that has spread to the lungs or liver.
MRI: An MRI can show whether cancer has spread to these areas. Sometimes contrast material makes abnormal areas show up more clearly on the picture.
Bone scan: The doctor injects a small amount of a radioactive substance into a blood vessel. It travels through the bloodstream and collects in the bones. A machine called a scanner detects and measures the radiation. The scanner makes pictures of the bones. Because higher amounts of the substance collect in areas where there is cancer, the pictures can show cancer that has spread to the bones.
PET scan: You’ll receive an injection of a small amount of radioactive sugar. The radioactive sugar gives off signals that the PET scanner picks up. The PET scanner makes a picture of the places in your body where the sugar is being taken up. Cancer cells show up brighter in the picture because they take up sugar faster than normal cells do.
Treatment and medication
These therapies may be used alone or in combination depending on the stage of the disease.
Surgery
This is the main treatment option which has not spread to other parts of the body and is also an option for more advanced stages of the disease. The types of breast cancer surgery differ in the amount of tissue that is removed with the tumour; this depends on the tumour’s characteristics, whether it has spread, and the patient’s personal feelings. Some of the most common types of surgery include:
‘Lumpectomy’ which involves the removal of the cancerous area, the surrounding tissue and in some cases the lymph node, whist aiming to maintain a normal breast appearance after surgery.
‘Partial Mastectomy’ or ‘Quadrantectomy’; this is where a larger portion of tissue is removed (compared with Lumpectomy)
‘Total Mastectomy’, which is performed in an attempt to further cancer prevention. This surgery involves the removal of the entire breast, without the removal of lymph nodes.
Radiotherapy
Therapy with radiation is often used in addition to surgery and chemotherapy to reduce the chances of the cancer recurring. It can be given after surgery (known as adjuvant treatment) or in conjunction with chemotherapy prior to surgery (neoadjuvant therapy) to shrink the tumour. Radiotherapy can also be used without surgery in patients with advanced metastatic breast cancer to help alleviate symptoms.
Chemotherapy
Chemotherapy may be given prior to surgery (neo-adjuvant) with the aim of reducing tumour size and the need for extensive surgery, or after surgery (adjuvant) to reduce the chances of the cancer coming back. When the cancer has spread to other parts of the body (metastatic), chemotherapy may be used to reduce symptoms, improve quality of life and extend survival.
Chemotherapy drugs can be given intravenously (directly into the blood), or orally in a tablet. Chemotherapy is typically associated with adverse side effects such as fatigue, nausea and diarrhea; this is because of its toxic nature and non-specific mode of action, which means that all cells are attacked (even healthy cells).
Hormonal therapy
Medicines that block or inhibit the actions of the hormones oestrogen and progesterone are often used in the treatment of patients with Hormone Receptor-Positive breast cancer.
Targeted therapy
Targeted therapies (also called biological therapies) are relatively new approach to cancer treatment and target specific biological processes that are often essential to tumour growth. Targeted therapy can include use of monoclonal antibodies, vaccines and gene therapies. Targeted therapies precisely target cancer-specific processes, making them effective and less toxic to non-cancerous, healthy cells. Several types of targeted therapy exist for the treatment of advanced stage. These are either given just after chemotherapy as maintenance or in conjunction with other therapies e.g. chemotherapies or hormonal therapies at various stages of advanced disease in accordance with their approved label.
Breast Reconstruction
A woman who plans to have a mastectomy has a choice about whether or not to have surgery to rebuild the shape of the breast (breast reconstruction). A surgeon can reconstruct the breast in many ways. Some women choose to have breast implants, which are filled with saline or silicone gel.
Early breast cancer prevention
Knowing whether or whether you have dense breasts is one of the most recent techniques to defend yourself. Younger women frequently have more tissue than fat in their breasts, which makes cancer difficult to detect on a mammogram: Breast tissue and cancers appear white, whereas fat appears dark.
Exercise appears to offer numerous defenses against it. It first aids in weight management.
Even your dad's cancer history is important to be aware of. Consult a genetics specialist if your family's medical history scares you.
Reduce the radiation that is exposed during screenings. Ionizing radiation, the kind used in numerous high-tech screening procedures, increases the risk of developing the disease because it can lead to DNA changes in cells.
Limit hormone therapy: Breast cancer risk is increased in women who utilize combination estrogen and progestin therapy over an extended period of time.
Take breastfeeding into consideration: For the first six months, women who continuously breastfeed have a 10% lower risk of dying from cancer.
Consume the right foods consistently. Harvard researchers recently discovered that women with blood carotenoid levels that were highest had a 19% lower risk of breast cancer than those with blood carotenoid levels that were lowest.
Find it early: The prognosis is frequently quite good when it is found early.
Thank you for reading this article please share with your friends and families. Enjoy your day.