In women who are in the reproductive stage, amenorrhea is the cessation of menstruation. However, it affects prepubescent, postmenopausal, and pregnant women frequently. Additionally, it stops in women who are nursing. Mensuration permanently ends around the age of 50. Instead of the disease, it is a health issue.
Amenorrhea types
Primary and Secondary amenorrhea are the two forms.
Basic amenorrhea
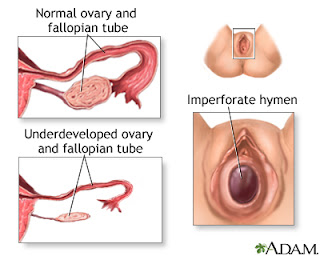
Primary amenorrhea is the term used to describe menstruation that does not start at puberty. If a patient has normal secondary sexual characteristics but has not reached menarche by the age of 16, primary amenorrhea can be identified. Primary amenorrhea can be identified as early as age 14 if a patient has neither menarche nor secondary sexual features.
Secondary amenorrhea
The cessation of menses for 3 months at any time after the menarche has occurred is referred to as secondary amenorrhea. This is normal during pregnancy, lactation, and menopausal age. Sometimes secondary amenorrhea may also occur for 6 months in women who already have normal periods. Secondary amenorrhea is the more common than the primary amenorrhea. Amenorrhea that occurs more than 9 months is called as oligomenorrhea.
Pathophysiology of amenorrhea
In general, the hypothalamus produces a series of a regulating hormone called gonadotropin-releasing hormone (GnRH). It stimulates the pituitary gland to release gonadotropins (follicle-stimulating hormone [FSH] and luteinizing hormone into the bloodstream. Under the stimulation of gonadotropins, ovaries produce androgens, estrogens, and progesterone and these perform different functions in the reproductive system as follows.
FSH: It stimulates the tissues of the reproductive organ which are particularly around the developing oocytes.
Oestrogen induces the endometrial lining and causes proliferation.
Leutinising hormone releases during the menstrual cycle to promote the maturation and release of the oocytes. Then to form the corpus luteum, which produces the hormone progesterone.
It changes the lining of the endometrium into a secretory structure and strengthens it for the implantation of the egg.
If the pregnancy does not take place, then the production of estrogen and progesterone decreases and thus the endometrium disrupted and shed during menses.
Epidemiology
No evidence indicates that the prevalence of amenorrhea varies according to national origin or ethnic group. However, local environmental factors related to nutrition and the prevalence of chronic disease undoubtedly have an effect.
For instance, the age of the first menses varies by geographic location, as demonstrated by a World Health Organization study comparing 11 countries, which reported a median age of menarche of 13-16 years across centers.
Natural causes: It can occur during pregnancy, lactation, and menopause stage of women.
Chromosomal or genetic abnormalities affect the function of ovaries and menstrual cycle. is Example: Turner syndrome
Problems with the hypothalamus or pituitary gland: It is an organ that regulates the releasing of gonadotropin-releasing hormone (GnRH), the hormone that starts the menstrual cycle. Pituitary tumors can also be a cause of amenorrhea.
Physical problems: Lack of reproductive organs and blockage of passages in the reproductive organs.
Gynecological conditions: Polycystic ovary syndrome (PCOS) and Fragile X-associated primary ovarian insufficiency (FXPOI),
Thyroid problems: Problem in the regulation of hormones by the thyroid gland. Hyperthyroidism and hypothyroidism cause irregularities in the menstrual cycle.
A family history of amenorrhea or early menopause
Some birth controls, such as pills, injections, or intrauterine devices. These can affect your menstrual cycle during and after use.
Medications: Antipsychotics, cancer chemotherapy, antidepressants, blood pressure drugs allergy medications.
Risk factors
Athletic training
Family history
Eating disorders
Women undertake high-volume/high-intensity exercise programs
Low fat, low carbohydrate diets
Use of anabolic steroids by female athletes is often responsible for a range of menstrual irregularities
Symptoms
The symptom of amenorrhea is the absence of menstrual cycle. You might experience symptoms other than the absence of menstrual cycle such as follows:
Milky discharge from breast who is not the pregnant (Galactorrhea) and changes in breast size
Reduced peripheral vision
Weight gain or weight loss may happen
Women may have psychological abnormalities with excessive anxiety
Vaginal dryness and pelvic pain
Increased hair growth in male pattern due to the androgen production
Acne and facial hair growth
Hair loss
Complications of amenorrhea
Some of the complications may arise such as:
Infertility ( ovulation doesn’t take place so you will not get pregnant)
Reduction in bone density cause weakness of bones (osteopenia or osteoporosis)
Diagnosis and test
First, your doctor may do the physical examination by examining the breast and genital area to see the normal changes in puberty.
Some of the following tests are carried out to determine the cause amenorrhea
Ultrasonography can be performed in pelvis area to determine the abnormalities in the genital tract or to check for polycystic ovary
MRI or CT scan of the head can be performed, to find out the pituitary and hypothalamic causes of amenorrhea
To determine the level of hormones secreted by the pituitary gland (FSH, LH, TSH, and prolactin) and the ovaries
The above tests are not indecisive to determine amenorrhea, the additional tests can be carried out such as:
Determination of prolactin level
Thyroid function tests
Uterus examination can be carried out by doing X-ray for hysterosalpingogram and saline infusion sonography
On the cause of the amenorrhea as well as the health status of the person. The primary amenorrhea is the late puberty so it doesn’t manage or treated. This condition will go off later. Some of the causes can be managed by drug therapies such as follows:
Dopamine agonist such as bromocriptine (Parlodel) or pergolide (Permax) is effective for treating hyperprolactinemia. It restores the normal endocrine function and ovulation
Metformin (Glucophage) to induce ovulation in women’s with polycystic ovary syndrome
In some cases, oral contraceptives may be prescribed to restore the menstrual cycle and to provide estrogen replacement to women with amenorrhea who do not wish to become pregnant. Before administering oral contraceptives, withdrawal bleeding is induced with an injection of progesterone or oral administration of 5-10 mg of medroxyprogesterone (Provera) for 10 days
Hormone replacement therapy can be used for the women who have low level of estrogen and progesterone
Some of the surgery options are preferred by the physician when in extreme cases such as
Surgery may require for someMensuration that does not occur at the puberty stage is referred as primary amenorrhea. Primary amenorrhea can be diagnosed if a patient has normal secondary sexual characteristics, but no menarche by 16 years of age. If a patient has no secondary sexual characteristics and no menarche, primary amenorrhea can be diagnosed as early as 14 years of age.
Additional amenorrhea
Secondary amenorrhea is the term used to describe the absence of menstruation for three months after the menarche. During pregnancy, nursing, and menopause, this is typical. Women who already have regular periods can experience secondary amenorrhea for a period of six months. Compared to initial amenorrhea, secondary amenorrhea is more frequent. Oligomenorrhea is the medical term for amenorrhea that lasts longer than nine months. depending on the unique clinical circumstance, are necessary for other genital tract problems.
Combating amenorrhea
By following procedures, a woman can stop amenorrhea from occurring.
logical exercise regimens
Preserving one's weight
Maintaining a healthy diet
Amenorrhea that is caused by genetics or by an inborn disease cannot be prevented.
Please share with your friends and families. Thank you.